It wasn’t “unreliable data”, it was outright and intentional fraud: the data NEVER existed in the first place. How many times have we been punked by criminal scientists? First, it was Covid itself. Then, it was HCQ. Then Ivermectin. Then, remdesivir (killed tens of thousands). Then, fraudulent hospital protocols that killed tens of thousands. This is a war against humanity perpetrated by monsters who are individually guilty of crimes against humanity. ⁃ Patrick Wood, TN Editor.
Early January of 2024, Americans learned about the publication of an article from Elsevier’s Journal of Biomedicine and Pharmacotherapy overseen by Dr. Danyelle Townsend, a professor at the University of South Carolina College of Pharmacy’s Department of Drug Discovery and Biomedical Sciences. As Editor-in-Chief, Dr. Townsend reviewed, approved, and published the article titled: “Deaths induced by compassionate use of hydroxychloroquine during the first COVID-19 wave: An estimate.”
The article was always a hypothesized estimate of people that might have died, but now even that estimate has been retracted. The reason for the retraction was that the Belgian dataset that was one of the bases for the piece was found to be “unreliable” (but in reality was fraudulent). The article also repeatedly referenced the New England Journal of Medicine’s 2020 RECOVERY trial. The RECOVERY trial is well known to be a deeply flawed study which, in addition to implementing late treatment in severely ill Covid patients, used extremely high doses of HCQ.
The now retracted publication authors were all French or Canadian, with the primary author a pharmacist by the name of Alexiane Pradelle. According to a rudimentary internet search, Dr. Pradelle had never published before. Subsequently, listed authors were degreed as physicians, pharmacists, and/or professors of their respective disciplines. The main, corresponding author, Jean-Christophe Lega, runs the Evaluation and Modeling of Therapeutic Effects team at the University of Lyon.
Hydroxychloroquine’s Fabled Safety History Contrasts Data
In addition to being a hypothesized estimate, the article also attacked the legendary safety of HCQ, contradicting centuries of the safety of quinolines as a class.
HCQ, chloroquine and quinine are structurally and pharmaceutically/mechanistically related, sharing the same quinoline structural group. The original iteration of quinine was a very fortunate discovery that dates back to the 1600s (at least) as a medicinal tipple used by Jesuit missionaries in South America. It is naturally found in the bark of the Cinchona tree (also called a “Quina-Quina” tree).
Quinine is still available today both as a prescription drug, for similar indications as HCQ including malaria…and as a Covid-19 treatment.
Quinine is so safe that it may be unique in that the FDA simultaneously permits its use without a prescription, as an ingredient in tonic waters.
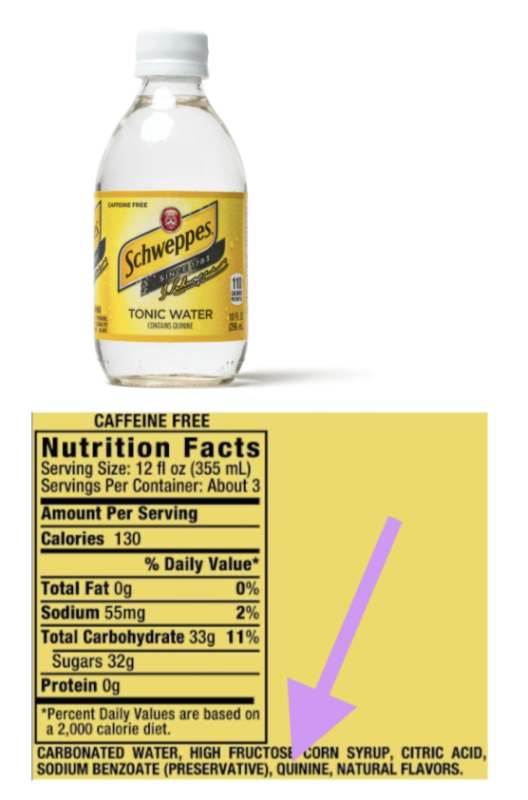
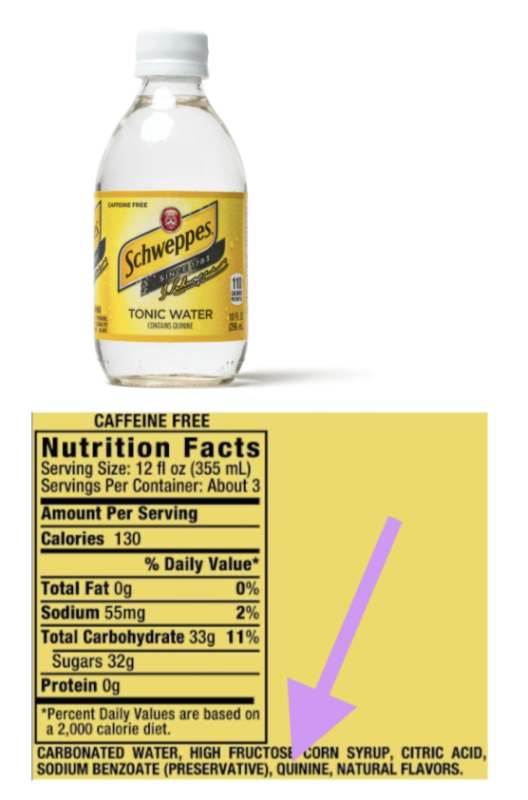
chweppes tonic water “Contains Quinine” as all tonic waters do. Winston Churchill once declared, “The gin and tonic has saved more Englishmen’s lives and minds than all the doctors in the Empire.”
HCQ is similarly safe when used appropriately and under medical supervision.
The CDC describes HCQ as “a relatively well tolerated medicine” and that “HCQ can be prescribed to adults and children of all ages. It can also be safely taken by pregnant women and nursing mothers” referring to its long-term use in chronic diseases.
Basic logic dictates that, if a drug is safe for long-term use, it would also be safe for short-term use, including (and especially) in Covid-19 early treatment/pre-exposure prophylaxis type indications.
These are pharmacology fundamentals that ought to be known by any pharmacist or physician – let alone to a professor serving as a Journal Editor-in-Chief at a taxpayer-funded state College of Pharmacy.
Did not even one person on her editorial board of over 50 “peer-reviewers” and staff ponder the celebrated and storied history of HCQ (and its predecessors) and how incongruent this study’s findings were before choosing to publish data denigrating HCQ safety?
The correct answer to that might actually be: “no”…
The publishing editorial board all seem to be laboratory bench (non-clinical) research scientists, per their biographies. Although the board does promote itself as meeting DEI requirements of being “gender diverse,” a more important question might be is if they have the appropriate credentials and experience to review and opine on clinically complex drug safety/epidemiology subject matters in the first place.
Is just anyone now allowed to opine on specialty clinical pharmacology drug safety matters?
In certain journals/news publications, the answer to that question seems to be: “yes”…
Those “17,000 Deaths” Never Occurred
Another point of confusion surrounded the interpretation and promotion of this little-known publication by the lay press.
To be exact: there were never “17,000 deaths;” it was always a hypothetical extrapolation of people that could have died, based on “unreliable” (eg, actually, fraudulent) databases on top of the previously mentioned, problematic late-stage RECOVERY-trial-type dosing and timing.
Still, Josh Cohen, a Forbes.com PhD senior healthcare columnist, used this publication to headline an absurdly biased op-ed against HCQ, stating that Trump’s HCQ proposal was “Linked To 17,000 Deaths.” Forbes’ Tufts, Harvard, and the University of Pennsylvania- trained “healthcare analyst” misrepresented or appeared to not understand the now-retracted study methodology or projections.
It went downhill from there. Mere hours following the publication, very similar, now objectively inaccurate, highly politicized, and seemingly coordinated attacks on HCQ and Trump were published by: The Hill, Politico, Frontline News, Scripps News, the Guardian, KFF Health News, News Nation, Newsweek, AOL.com, Yahoo News, and Daily Kos, in addition to a multitude of prominent regional, international, and US federal news outlets, many falsely estimating that 17,000 deaths had already taken place and that the (imaginary) victims’ blood was already on Donald Trump’s hands.
As of September 15, 2024, the above and other articles still show up very prominently (on the first page) of a Google search for “hydroxychloroquine deaths”…which never happened.
Here are some screenshots of headlines referencing non-existent deaths based on a now-retracted study:


As of September 19, these headlines are all on the first page of a Google search for “hydroxychloroquine deaths.”








Journal Editors Were Immediately Warned about Questionable Findings
Almost immediately following the January 2, 2024 publication, its critical flaws including basic miscalculations among many other deficiencies were brought to the attention of Dr. Townsend by Xavier Azalbert and non-profit BonSens.org attorneys starting on Jan 7, 2024. In fact, a total of 9 communications were sent by the above individuals, but none of them were ever shared as “Letters to The Editor” by Dr. Townsend in good faith to inform readers of specific potential shortcomings, as is otherwise commonly done.
Dr. Townsend seemed to forget that bad medical data and publications can do actual patient harm, and kept legitimate and important study criticisms to herself. Instead of taking responsibility and making a leadership decision, she passed the buck to a Committee on Publication Ethics, delaying the needed retraction.
It appallingly took 234 days (~7 months, from the January 2nd publication to August 26th) for Dr. Townsend’s Journal of Biomedicine and Pharmacotherapy to finally retract the “unreliable” article. But at that point, untold millions around the world had already been (and continue to be) polluted with outrageously incorrect information about non-existent HCQ deaths.
This raises some questions about Dr. Townsend’s duties and responsibilities as the Editor in Chief:
- What efforts were made to correct incorrect headlines and articles published by the lay press, incorrectly frightening patients, pharmacists, and physicians, by fueling false tropes about HCQ?
- What efforts were made to let news organizations know that data from the peer-reviewed publication was under question? (She refers to “a number of Letters to the Editor and correspondence from readers.”)
- What immediate efforts are being made to notify news organizations and/or amplify search engine results regarding the now-retracted publication?
- What funding source/individual paid the $3,490 (“excluding taxes and fees”) publication fee? (Note: reputable academic journals do not charge to publish articles.)
- Does Elsevier’s Journal of Biomedicine and Pharmacotherapy meet certain definitions of what is known as a predatory publisher?
- Was this Editorial Board qualified to review regulatory/drug safety/epidemiology/any other clinical subjects?
- Are the ramifications of this Journal’s publication and its subsequent retraction known to the University of South Carolina administration, co-faculty, and whichever body adjudicates its faculty Code of Ethics & Standards of Practice?
- This isn’t the first time Townsend has needed to retract articles – a normally very rare occurrence for reputable journals. Will Elsevier, which publishes over 2,700 journals, permit further opining or publishing on clinical subjects by this editorial board? Can the Editor-in-Chief and/or editorial board be trusted to recuse themselves from opining on any topics that are not within their area of expertise?
- What should be done to prevent a reoccurrence of this incident at the University of South Carolina and other taxpayer-funded institutions?
Beyond that, what ramifications/punishments (if any) will occur for other prominent Covid-19 Lancet and New England Journal of Medicine authors/publishers whose articles were also retracted after they were found to be based on so-called “unreliable” (eg, non-existent) databases?
Ethical scientists who believe in truth, transparency, and academic accountability are standing by, waiting for medical and academic justice.
Unethical scientists are also watching this situation unfold, twisting their mustaches, learning about what they could potentially one day get away with.
Read full story here…










