Cytotoxic T lymphocytes play a crucial role in adaptive immunity, primarily defending against tumors and viruses. These cells develop within the thymus gland and undergo rapid activation upon encountering an antigen.
Some T-cells also form memory T lymphocytes, which are affected by in vivo environments and host factors. Understanding the molecular basis of exhausted and memory T lymphocytes is essential to develop cell-mediated immunity-based interventions.
In a recent review published in Cellular & Molecular Immunology, researchers describe molecular signaling regulated by mammalian target of rapamycin (mTOR), especially mTOR complex 2 (mTORC2), among memory and exhausted cytotoxic cluster of differentiation 8-expressing (CD8+) T lymphocytes.
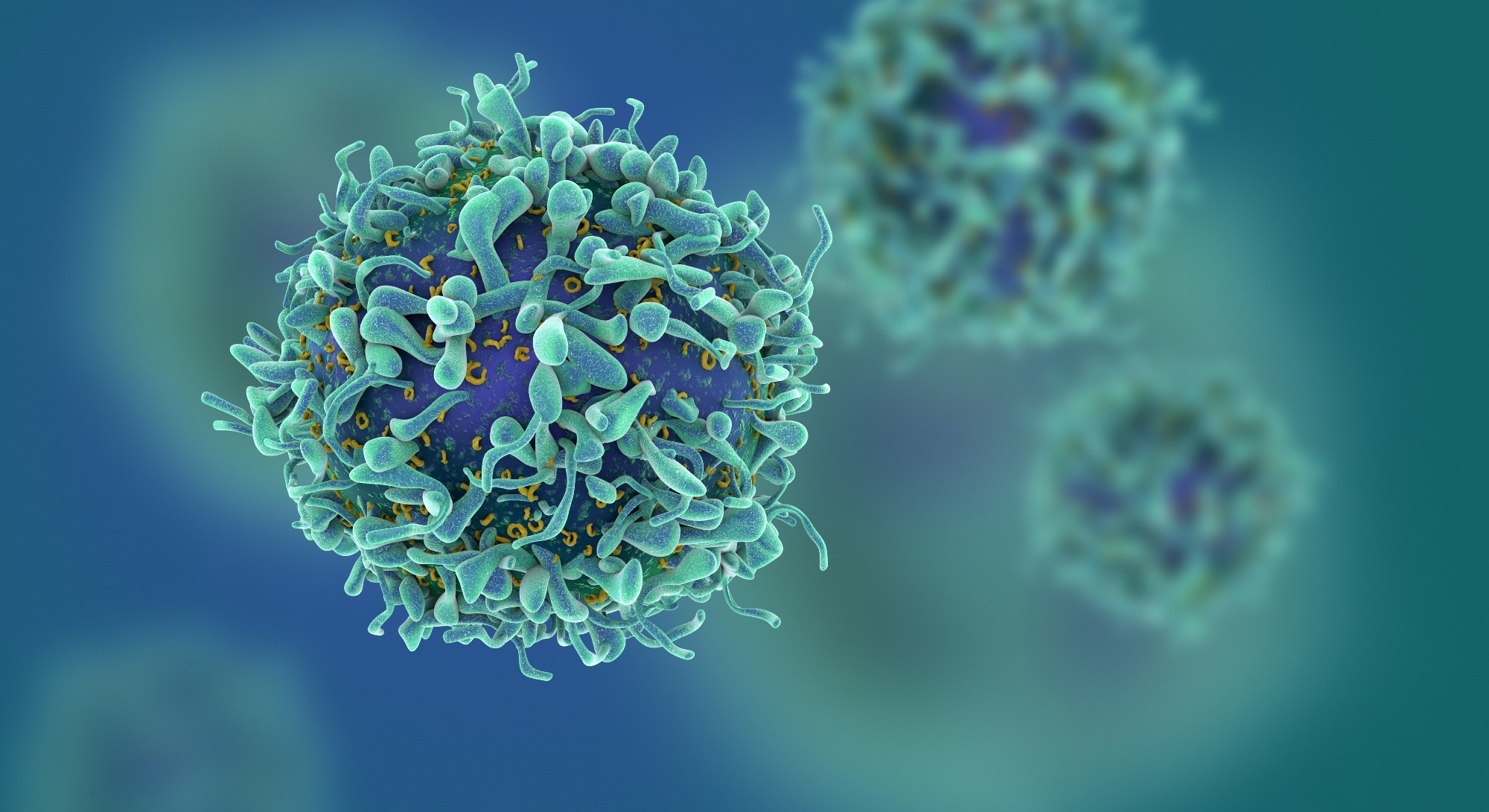 Study: Regulation of CD8+ T memory and exhaustion by the mTOR signals. Image Credit: fusebulb / Shutterstock.com
Study: Regulation of CD8+ T memory and exhaustion by the mTOR signals. Image Credit: fusebulb / Shutterstock.com
Integration of cellular metabolic pathways by mTOR and mechanisms underlying T lymphocyte exhaustion
Cytotoxic T cells (CTLs) differentiate to form effector cells in acute infections and memory cells for durable immune protection. In chronic infections and cancer, CTLs progressively differentiate into a dysfunctional exhaustive state.
The immune system’s complex nature is highlighted by the heterogeneous pools of exhausted and memory CTLs. Chronic antigen stimulation and inflammation can lead to T-cell exhaustion, which is characterized by loss of effector function and expression of multiple inhibitory receptors.
T-cell receptor (TCR) stimulation is the major cause of T lymphocyte exhaustion, with exhausted (Tex) cells constituting a unique cytotoxic subset. Tex cells produce lower levels of cytokines and fewer cytotoxic effector molecules.
The pool of exhausted cytotoxic T lymphocytes is diverse and comprises distinct subsets. During chronic infection or tumor growth, these cells become progenitor-exhausted T lymphocytes (progenitor Tex cells), with high Ly108 expression and low CX3C motif chemokine receptor 1 (CX3CR1) and killer cell lectin-like receptor G (KLRG) expression. TCR signaling activates downstream transcription factors (TFs), thereby boosting progenitor Tex cell differentiation into Tex cells.
Naïve cytotoxic T lymphocytes are quiescent and rely on oxidative phosphorylation (OXPHOS) in mitochondria. When activated, these cells undergo metabolic reprogramming, thus triggering aerobic glycolysis and oxidative phosphorylation (OXPHOS) pathways for rapid cellular growth and proliferation.
Effector cells primarily undergo aerobic glycolysis, while memory cytotoxic T-cells exhibit enhance OXPHOS and fatty acid oxidation. Chronic infection or tumorigenesis impairs major metabolic pathways, thereby making Tex cells highly dependent on glycolysis.
Role of mTOR signaling in cytotoxic T-cell differentiation
The activity of mTOR complexes, mTORC1, and mTORC2, differentially dictates cytotoxic T lymphocyte fate and memory T lymphocyte formation. Moreover, mTORC1 controls cell development and metabolism, whereas mTORC2 controls cell viability and cytoskeletal architecture. The mTOR complexes regulate each other through S6K phosphorylation and TSC complex inhibition.
During vaccination and acute infection, effector CD8+ T lymphocytes differentiate to form two distinct subsets, including short-lived effector cells (SLECs) and memory precursor effector cells (MPECs) with similar cytotoxic effector functions. After the effector phase ends or after antigen clearance, the majority of SLECs undergo apoptosis, with only a few surviving to form long-lived effector cells (LLEs).
MPECs differentiate to form central memory T (Tcm), residential memory T (Trm), and effector memory T (Tem) lymphocytes. The Sin1/mTORC2 complex may directly regulate the GATOR1-KICSTOR complex, controlling cell growth, metabolism, immune responses, and tumorigenesis.
Rapamycin treatment induces the MPEC phenotype by antigen-specific cytotoxic T-cells to ensure the survival and differentiation of memory precursor T-cells. Early treatment increases progenitor Tex cells, reduces Tex cells, and increases proliferation, ultimately enhancing anti-programmed cell death ligand 1 (PD-L1) therapy efficacy. Sin1, a mTOR component, is crucial for T lymphocyte maturation, cytokine production, and immune niche regulation.
Downregulation of mTORC1 and mTORC2 signaling facilitates antibacterial immunity after diet restriction. In fact, mTOR regulates cytotoxic T lymphocyte fate by regulating TF expression, Eomes, and T-bet, all of which are crucial for CTL and immunological memory during infection. Interleukin-12 (IL-12) promotes effector cell production by inhibiting Eomes and promoting T-bet expression.
IL-12-induced signal transducer and activator of transcription 4 (STAT4) signaling pathways enhance mTOR activity, whereas rapamycin treatment upregulates Eomes expression. Additionally, mTORC1/mTORC2 in cytotoxic T lymphocytes influence metabolic pathways, with effector cells undergoing aerobic glycolysis and memory cells displaying enhanced OXPHOS and fatty acid oxidation. Three generations of mTOR inhibitors have been developed for cell growth and metabolic control.
Conclusions
Based on the review findings, mTOR has a crucial role in regulating T lymphocyte function, including their development, activation, differentiation, migration, survival, memory formation, and exhaustion. Understanding the heterogeneity and diversity of memory and exhaustion cytotoxic T-lymphocyte subsets is essential for adaptive immunity.
Further research is needed to elucidate molecular mechanisms regulating cytotoxic T-cell fate and evaluate the mTOR as a molecular target for modulating cellular metabolism and enhancing exhausted T lymphocyte function.









