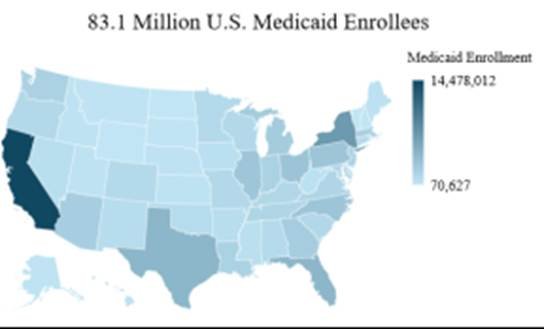
Reduced Medicaid spending as a result of the One Big Beautiful Bill Act will create a more complex and challenging near-term environment for municipal bond investors.
The United States not-for-profit hospital sector has spent much of the post-COVID period navigating a fragile rebound. According to Moody’s recent Medians report, fiscal 2024 marked a year of improvement. Revenues rose faster than still elevated expenses, supported by recovering patient volumes.
Yet the relief has been tempered by structural shifts that lie ahead. The passage of the One Big Beautiful Bill Act (OBBBA) introduces policy changes that could reshape financial performance and challenge investors’ assumptions.
Policy changes on the horizon
At the center of the OBBBA are provisions aimed at reducing Medicaid spending. These measures include stricter eligibility recertifications, new work requirements, and caps on provider taxes and state-directed payments. The legislation also restricts Affordable Care Act marketplace eligibility and permits ACA premium tax credits to expire at the end of 2025. Such changes are likely to result in higher premiums and may lead some households to drop their coverage.

Source: Internal, KFF.org
The Congressional Budget Office estimates that the OBBBA will reduce federal Medicaid spending by $911 billion over ten years and increase the number of uninsured individuals by 10 million. In rural areas, federal Medicaid support is projected to decline by $137 billion, compared with $50 billion appropriated for the rural health fund. The bulk of these changes are scheduled to begin in 2027, a point at which many hospitals will still be consolidating their post-pandemic recovery.
Sector structure and vulnerability
Of the 6,093 hospitals in the United States, 84% are community hospitals, and 58% of those are non-profit. In 2023, private health insurance accounted for 37% of hospital spending, Medicare accounted for 25%, and Medicaid accounted for 19%. Private insurance includes both employer-sponsored plans and coverage purchased through the Affordable Care Act marketplace.
The pressures on the sector are not evenly distributed. Rural hospitals remain especially vulnerable. Over the past two decades, roughly 200 rural hospitals have closed. Almost half of those that remain operate at a loss, and closures in rural areas continue to outpace those in urban areas by a factor of four to one. Reductions in Medicaid support would amplify these pressures.
Implications for bond investors
For municipal bond investors, the sector presents both risks and points of differentiation. Standard and Poor’s rates approximately 450 hospitals across the country. The Bloomberg Municipal Bond Index includes 358 unique hospital issuers with more than $163 billion in par outstanding, making it the second-largest sector in the index by par value.
Future stress points are already visible. Rising uninsured rates are expected to emerge in 2026 and 2027, creating additional pressure on profitability and balance sheets. Some smaller, standalone, and county-owned hospitals may not be able to withstand the financial strain and could close or merge into larger systems. Larger health systems with more diversified payer mixes and stronger balance sheets may demonstrate greater resilience, but they too will need to adjust to the shifting reimbursement landscape.

Source: Internal, Bloomberg LMBITR Index
Looking ahead
As federal policies change, the operating landscape for not-for-profit hospitals will become more challenging. For investors, key factors will include credit fundamentals such as payer mix, scale, cost structure, and regional demographics. The ability to distinguish between stronger and weaker issuers will become increasingly crucial.
The outlook is not simply a recovery or decline. It is a landscape shaped by uneven pressures and resilience, where understanding credit fundamentals will remain vital for making investment decisions.
Jude Scaglione is the director and head of municipal credit research at Alvarez & Marsal Private Wealth Partners.